If you read any research about Alzheimer’s disease, two proteins are going to be your main characters. There’s amyloid-β, which builds up and forms plaques in the brain; and there’s tau, which aggregates into clumps called tangles. These tangles occur when the tau protein is altered by phosphorylation, and for many decades, the buildup of phosphorylated tau (p-tau) has been considered a biomarker of Alzheimer’s disease.
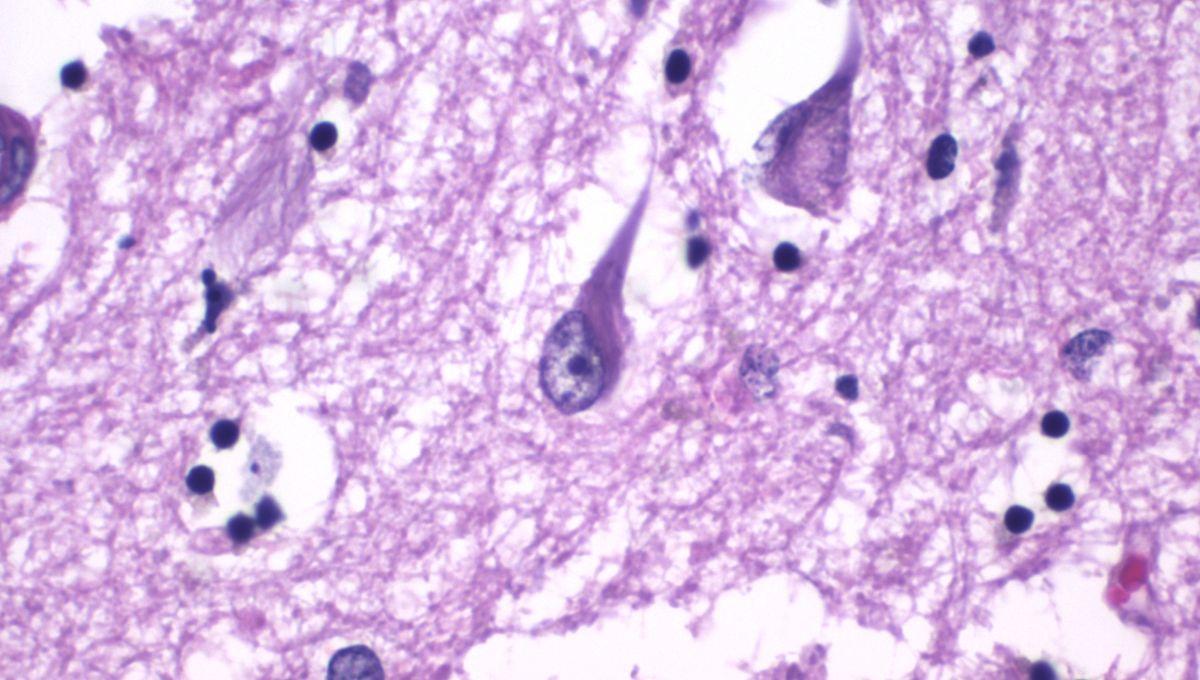
You can imagine researchers’ surprise, then, when they discovered levels of p-tau that far outstrip those in typical Alzheimer’s patients in possibly the most unlikely subjects of all: newborn babies. In a new paper, researchers led by Fernando Gonzalez-Ortiz, MD, PhD of the University of Gothenburg (@Rantes_) lay out their paradoxical findings after analyzing samples from 462 newborn and premature infants, Alzheimer’s patients, and healthy controls. They found that plasma p-tau levels were consistently elevated in newborns compared with any other age group, and exceeded the levels seen in patients with Alzheimer’s. We tend to think of p-tau as a toxic and bad thing. Fernando Gonzalez-Ortiz Intrigued to find out more, IFLScience sat down with Gonzalez-Ortiz and started by asking him how the study came about. “That is such a funny story,” he told us. “Three years ago, we got CSF [cerebrospinal fluid] samples from newborns where the paediatrician suspected intraventricular bleeding. […] I was like, ‘Wait, why don’t we check levels of p-tau in these CSF samples?’ So then I measured the standard biomarkers […] and all of them were incredibly high.” By “incredibly high”, Gonzalez-Ortiz explained that that meant 20 times higher in some cases. Despite interest from colleagues over these striking findings, there was some concern that the results could be anomalous because the babies in the sample all had significant medical issues. And so, the team essentially bided their time, until another group of samples became available. This time, they were able to test cord blood samples from healthy newborns and compare their results with analyses of patients with Alzheimer’s – and they replicated their initial findings. “Now we know that this is true. Now we know that it’s higher [in newborns] than Alzheimer’s disease. The question is, when does it go down?” The last piece of the puzzle for the current study was found when the team got access to data from a cohort of premature infants. Since they remained in hospital for a period of time, there was a set of blood samples available for each patient, providing a crucial longitudinal view of their clinical condition. While the findings are preliminary, and Gonzalez-Ortiz was quick to stress that the study has many limitations, at the very least it shows us that some of our assumptions about tau have been wrong. “P-tau has always been seen as this purely [Alzheimer’s disease] biomarker,” he explained. This has meant less attention has been paid to its possible physiological roles, and how levels may fluctuate over the course of someone’s life. “We tend to think of p-tau as a toxic and bad thing, and that seems to be the case in Alzheimer’s disease. But the question is, what happens in the developing brain that actually somehow handles the high concentrations of p-tau? If we manage to understand more what happens in the brains of newborns, we might be able to create more physiological therapies for Alzheimer’s.” Recent years have seen the approval of a wave of new drugs for Alzheimer’s disease. These have all targeted the other protein big hitter that we mentioned, amyloid-β. Drugs like lecanemab and donanemab have garnered a lot of attention. While some have hailed them as breakthroughs, others have cast doubt on their effectiveness. The first of this new class of drug to be approved, aducanumab, was actually discontinued in 2024, though manufacturer Biogen stated that this was a business decision as opposed to an indication that the drug didn’t work. None of these drugs claim to cure the disease either, though they may slow its progression. On top of that, the entire “amyloid hypothesis” has been called into question and the field has been mired in controversy in recent years. Other avenues are being explored, including vaccine candidates for Alzheimer’s, but this paper from Gonzalez-Ortiz and the team could be taken as an indication – as others have argued – that the focus on amyloid has been myopic, and that it’s time for more research energy to be invested in tau. “We know that the main driver of cognitive decline in Alzheimer’s disease is actually tau accumulation and tau tangles,” Gonzalez-Ortiz told IFLScience. These biomarkers are not just there to tell you who has Alzheimer’s disease or not. Fernando Gonzalez-Ortiz Going forward, he told us his major ambitions for this research include bringing on collaborators to launch a larger project, which could explore whether p-tau is a useful biomarker in newborns – could it be that those with the highest levels at birth are more likely to develop Alzheimer’s in the future? Could it be correlated with other neurological conditions? What about people with familial Alzheimer’s, who tend to develop symptoms at a much younger age. We simply don’t know yet. It’s also unclear whether the patterns of tau phosphorylation in newborns mirror those in Alzheimer’s patients, or if there are some biologically important differences there. One theory is that higher p-tau levels may allow the brain to generate new synaptic connections, and that the high levels seen in babies are a function of the spurt of neurodevelopment they’re experiencing. If that’s the case, Gonzalez-Ortiz theorized, “then does this mean that at certain points in life where we know that there is an important development in the brain of the individual, do the levels rise again?” Aggregates of tau protein are shown in light blue inside magenta microtubules in this model of tau pathology. Image credit: Melina Gyparaki, Melike Lakadamyali’s lab, Perelman School of Medicine at the University of Pennsylvania via Flickr (public domain) But a key message that Gonzalez-Ortiz stressed to us is that it can be too easy to get laser-focused on all these proteins and forget the wider context – especially with a newly approved test for p-tau 217, one of the strongest Alzheimer’s biomarkers we’re aware of. “People […] believe that 217 equals Alzheimer’s disease. The thing we need to understand is that without proper clinical context, biomarker levels don’t mean anything.” “We use the biomarker as a way to understand the disease, but […] these biomarkers are not just there to tell you who has Alzheimer’s disease or not.” Viewed through that lens, the presence in newborn baby brains of hugely high levels of a protein that was long thought to indicate Alzheimer’s disease becomes less shocking, and much more curious. We left our conversation with Gonzalez-Ortiz with many more questions, but this is one field of research we’ll be keen to follow in the coming years. “It’s like the alpha and omega,” he mused. “During foetal life you have this super important process, and then Alzheimer’s disease is the most common cause of dementia, so for many individuals this is the end of their life. It’s the final stage. And in both cases, phosphorylation of tau plays a massive role in development – in the construction and in the destruction of the brain.” The study is published in the journal Brain Communications. Tau: time for another look?